|
What is Fecal Incontinence ?
Fecal incontinence is the
inability to control your bowels. When you feel the urge to have a
bowel movement, you may not be able to hold it until you get to a
toilet. Or stool may leak from the rectum unexpectedly, sometimes
while passing gas.
More than 5.5 million Americans have fecal incontinence. It
affects people of all agesóchildren and adults. Fecal incontinence
is more common in women and older adults, but it is not a normal
part of aging.
Loss of bowel control can be devastating. People who have fecal
incontinence may feel ashamed, embarrassed, or humiliated. Some
donít want to leave the house out of fear they might have an
accident in public. Most try to hide the problem as long as
possible, so they withdraw from friends and family. The social
isolation is unfortunate but may be reduced with treatment that
improves bowel control and makes incontinence easier to manage.
What causes fecal incontinence?
Fecal incontinence can have several causes:
* constipation
* damage to the anal sphincter muscles
* damage to the nerves of the anal sphincter muscles or the rectum
* loss of storage capacity in the rectum
* diarrhea
* pelvic floor dysfunction
Constipation
Constipation is one of the most common causes of fecal
incontinence. Constipation causes large, hard stools to become
lodged in the rectum. Watery stool can then leak out around the
hardened stool. Constipation also causes the muscles of the rectum
to stretch, which weakens the muscles so they canít hold stool in
the rectum long enough for a person to reach a bathroom.
Muscle Damage
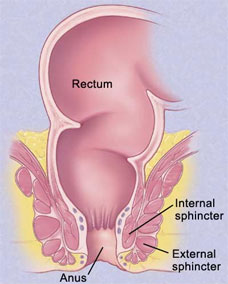
Fecal incontinence can be caused by injury to one or both of the
ring-like muscles at the end of the rectum called the anal
internal and external sphincters. The sphincters keep stool
inside. When damaged, the muscles arenít strong enough to do their
job and stool can leak out. In women, the damage often happens
when giving birth. The risk of injury is greatest if the doctor
uses forceps to help deliver the baby or performs an episiotomy,
which is a cut in the vaginal area to prevent it from tearing
during birth. Hemorrhoid surgery can also damage the sphincters.
Nerve Damage
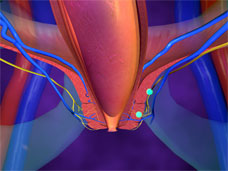
Fecal incontinence can be caused by damage to the nerves that
control the anal sphincters or the nerves that sense stool in the
rectum. If the nerves that control the sphincters are injured, the
muscles donít work properly and incontinence can occur. If the
sensory nerves are damaged, they donít sense that stool is in the
rectum so you wonít feel the need to use the bathroom until stool
has leaked out. Nerve damage can be caused by childbirth, a
long-term habit of straining to pass stool, stroke, physical
disability due to injury, and diseases that affect the nerves such
as diabetes and multiple sclerosis.
Loss of Storage Capacity
Normally, the rectum stretches to hold stool until you can get to
a bathroom. But rectal surgery, radiation treatment, and
inflammatory bowel disease can cause scarring that makes the walls
of the rectum stiff and less elastic. The rectum then canít
stretch as much to hold stool and fecal incontinence results.
Inflammatory bowel disease also can irritate rectal walls, making
them unable to contain stool.
Diarrhea
Diarrhea, or loose stool, is more difficult to control than solid
stool because with diarrhea the rectum fills with stool at a
faster rate. Even people who donít have fecal incontinence can
leak stool when they have diarrhea.
Pelvic Floor Dysfunction
Abnormalities of the pelvic floor muscles and nerves can cause
fecal incontinence. Examples include
* impaired ability to sense stool in the rectum
* decreased ability to contract muscles in the anal canal to
defecate
* dropping down of the rectum, a condition called rectal prolapse
* protrusion of the rectum through the vagina, a condition called
rectocele
* general weakness and sagging of the pelvic floor
Childbirth is often the cause of pelvic floor dysfunction, and
incontinence usually doesnít appear until the midforties or later.
How is fecal incontinence diagnosed?
Doctors understand the feelings associated with fecal
incontinence, so you can talk freely with your doctor. The doctor
will ask some health-related questions, do a physical exam, and
possibly run some medical tests. Your doctor may refer you to a
specialist, such as a gastroenterologist, proctologist, or
colorectal surgeon.
The doctor or specialist may conduct one or more tests:
Anal manometry checks the tightness of the anal sphincter and its
ability to respond to signals, as well as the sensitivity and
function of the rectum. Magnetic resonance imaging (MRI) is
sometimes used to evaluate the sphincter.
Anorectal ultrasonography evaluates the structure of the anal
sphincters.
Proctography, also known as defecography, shows how much stool the
rectum can hold, how well the rectum holds it, and how well the
rectum can evacuate it.
Proctosigmoidoscopy allows doctors to look inside the rectum and
lower colon for signs of disease or other problems that can cause
fecal incontinence, such as inflammation, tumors, or scar tissue.
Anal electromyography tests for nerve damage, which is often
associated with injury during childbirth.
How is fecal incontinence treated?
Effective treatments are available for fecal incontinence and can
improve or restore bowel control. The type of treatment depends on
the cause and severity of fecal incontinence; it may include
dietary changes, medication, bowel training, or surgery. More than
one treatment may be necessary for successful control because
continence is a complicated chain of events.
Dietary Changes
Food affects the consistency of stool and how quickly it passes
through the digestive system. If your stools are hard to control
because they are watery, you may find that eating high-fiber foods
adds bulk and makes stool easier to control. But people with
well-formed stools may find that high-fiber foods act as a
laxative and contribute to the problem. Foods and drinks that may
make the problem worse are those containing caffeineólike coffee,
tea, or chocolateówhich relaxes the internal anal sphincter
muscles.
You can adjust what and how you eat to help manage fecal
incontinence.
Keep a food diary. List what you eat, how much you eat, and when
you have an incontinent episode. After a few days, you may begin
to see a pattern involving certain foods and incontinence. After
you identify foods that seem to cause problems, cut back on them
and see whether incontinence improves. Foods and drinks that
typically cause diarrhea, and so should probably be avoided,
include
o drinks and foods containing caffeine
o cured or smoked meat such as sausage, ham, or turkey
o spicy foods
o alcoholic beverages
o dairy products such as milk, cheese, or ice cream
o fruits such as apples, peaches, or pears
o fatty and greasy foods
o sweeteners, such as sorbitol, xylitol, mannitol, and fructose,
which are found in diet drinks, sugarless gum and candy,
chocolate, and fruit juices
*
Eat small meals more frequently. In some people, large meals cause
bowel contractions that lead to diarrhea. You can still eat the
same amount of food in a day, but space it out by eating several
small meals.
*
Eat and drink at different times. Liquid helps move food through
the digestive system. So if you want to slow things down, drink
something half an hour before or after meals, but not with meals.
*
Eat the right amount of fiber. For many people, fiber makes stool
soft, formed, and easier to control. Fiber is found in fruits,
vegetables, and grains, like those listed below. You need to eat
20 to 30 grams of fiber a day, but add it to your diet slowly so
your body can adjust. Too much fiber all at once can cause
bloating, gas, or even diarrhea. Also, too much insoluble, or
undigestible, fiber can contribute to diarrhea. If you find that
eating more fiber makes your diarrhea worse, try cutting back to
two servings each of fruits and vegetables and removing skins and
seeds from your food.
*
Eat foods that make stool bulkier. Foods that contain soluble, or
digestible, fiber slow the emptying of the bowels, including
bananas, rice, tapioca, bread, potatoes, applesauce, cheese,
smooth peanut butter, yogurt, pasta, and oatmeal.
*
Get plenty to drink. Drink eight 8-ounce glasses of liquid a day
to help prevent dehydration and keep stool soft and formed. Water
is a good choice. Avoid drinks with caffeine, alcohol, milk, or
carbonation if you find they trigger diarrhea.
Over time, diarrhea can keep your body from absorbing vitamins and
minerals. Ask your doctor if you need a vitamin supplement.
|