| |
 |
|
|
|
|
|
Biliary Atresia |
|
|
What is biliary atresia?
Biliary atresia is a serious but rare disease of the
liver that affects newborn infants. It occurs in about one in
10,000 children and is more common in girls than in boys and in
Asian and African-American newborns than in Caucasian newborns.
The cause of biliary atresia is not known, and treatments are only
partially successful.
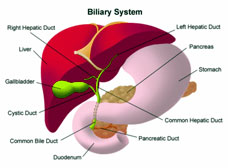
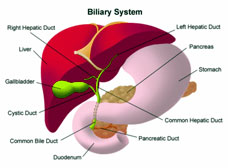
The liver damage incurred from biliary atresia is caused by injury
and loss (atresia) of the bile ducts that are responsible for
draining bile from the liver. Bile is made by the liver and passes
through the bile ducts and into the intestines where it helps
digest food, fats, and cholesterol. The loss of bile ducts causes
bile to remain in the liver. When bile builds up it can damage the
liver, causing scarring and loss of liver tissue. Eventually the
liver will not be able to work properly and cirrhosis will occur.
Once the liver fails, a liver transplant becomes necessary.
Biliary atresia can lead to liver failure and the need for liver
transplant within the first 1 to 2 years of life.
What are the symptoms of biliary atresia?
The first sign of biliary atresia is jaundice, which causes a
yellow color to the skin and to the whites of the eyes. Jaundice
is caused by the liver not removing bilirubin, a yellow pigment
from the blood. Ordinarily, bilirubin is taken up by the liver and
released into the bile. However, blockage of the bile ducts causes
bilirubin and other elements of bile to build up in the blood.
Jaundice may be difficult for parents and even doctors to detect.
Many healthy newborns have mild jaundice during the first 1 to 2
weeks of life due to immaturity of the liver. This normal type of
jaundice disappears by the second or third week of life, whereas
the jaundice of biliary atresia deepens. Newborns with jaundice
after 2 weeks of life should be taken to the doctor to check for a
possible liver problem.
Other signs of jaundice are a darkening of the urine and a
lightening in the color of bowel movements. The urine darkens from
the high levels of bilirubin in the blood spilling over into the
urine, while stool lightens from a lack of bilirubin reaching the
intestines. Pale, grey, or white bowel movements after 2 weeks of
age are probably the most reliable sign of a liver problem and
should prompt a visit to the doctor.
What causes biliary atresia?
The cause of biliary atresia is not known. The two types of
biliary atresia appear to be a “fetal” form, which arises during
fetal life and is present at the time of birth, and a “perinatal”
form, which is more typical and does not become evident until the
second to fourth week of life. Some children, particularly those
with the fetal form of biliary atresia, often have other birth
defects in the heart, spleen, or intestines.
An important fact is that biliary atresia is not an inherited
disease. Cases of biliary atresia do not run in families;
identical twins have been born with only one child having the
disease. Biliary atresia is most likely caused by an event
occurring during fetal life or around the time of birth.
Possibilities for the “triggering” event may include one or a
combination of the following factors:
* infection with a virus or bacterium
* a problem with the immune system
* an abnormal bile component
* an error in development of the liver and bile ducts
Research on the cause of biliary atresia is of great importance.
Progress in the management and prevention of biliary atresia can
only come from a better understanding of its cause or causes.
How is it diagnosed?
Worsening jaundice during the first month of life means a liver
problem is present. The specific diagnosis of biliary atresia
requires blood and x-ray tests, and sometimes a liver biopsy. If
biliary atresia is suspected, the newborn is usually referred to a
specialist such as
* a pediatric gastroenterologist who is an expert in digestive
diseases of children
* a pediatric hepatologist who is an expert in liver disease of
children
* a pediatric surgeon who specializes in surgery of the liver and
bile ducts
Initial tests. The doctor will press on the baby’s abdomen to
check for an enlarged liver or spleen and order blood, urine, and
stool tests to check for liver problems. The level of bilirubin in
the blood will be measured and special tests for other causes of
liver problems will be done.
Ultrasound of the abdomen and liver. Ultrasound tests produce an
image on a computer screen using sound waves. Ultrasound tests can
show whether the liver or bile ducts are enlarged and whether
tumors or cysts are blocking the flow of bile. An ultrasound
cannot be used to make a diagnosis of biliary atresia, but it does
help rule out other common causes of jaundice.
Liver scans. Liver scans are special types of x rays that use
substances that can be detected by cameras to create an image of
the liver and bile ducts. One such test is called hepatobiliary
iminodiacetic acid (HIDA) scanning. HIDA scans trace the path of
bile in the body and can show whether bile flow is blocked.
Liver biopsy. If another medical problem is not found to be the
cause of jaundice, a liver biopsy may be recommended. For a liver
biopsy, the infant is sedated and a needle is passed through the
skin and then quickly in and out of the liver. A small piece of
liver, about the size of a pencil lead, is obtained for
examination using a microscope. A liver biopsy will usually show
whether biliary atresia is likely. A biopsy can also help rule out
other liver problems, such as hepatitis.
How is it treated?
Surgery. If biliary atresia appears to be the cause of the
jaundice in the newborn, the next step is surgery. At the time of
surgery the bile ducts can be examined and the diagnosis
confirmed. For this procedure, the infant is sedated. While the
infant is asleep, the surgeon makes an incision in the abdomen to
directly examine the liver and bile ducts. If the surgeon confirms
that biliary atresia is the problem, a Kasai procedure will
usually be performed on the spot.
Kasai procedure (hepato-portoenterostomy). If biliary atresia is
the diagnosis, the surgeon generally goes ahead and performs an
operation called the “Kasai procedure,” named after the Japanese
surgeon who developed this operation. In the Kasai procedure, the
bile ducts are removed and a loop of intestine is brought up to
replace the bile ducts and drain the liver. As a result, bile
flows from the small bile ducts straight into the intestine,
bypassing the need for the larger bile ducts completely. (More
about the Kasai procedure follows.)
Liver transplant. If the Kasai procedure is not successful, the
infant usually will need a liver transplant within the first 1 to
2 years of life. Children with the fetal form of biliary atresia
are more likely to need liver transplants—and usually sooner—than
infants with the typical perinatal form. The pattern of the bile
ducts affected and the extent of damage can also influence how
soon a child will need a liver transplant. (More about liver
transplantation follows.)
The Kasai Procedure
The Kasai procedure can restore bile flow and correct many of the
problems of biliary atresia. This operation is usually not a cure
for the condition, although it can have an excellent outcome.
Without this surgery, a child with biliary atresia is unlikely to
live beyond the age of 2. The operation works best if done before
the infant is 90 days old and results are usually better in
younger children.
The improved results of the surgery make the early diagnosis of
biliary atresia very important, preferably before the infant is
several months old and has suffered permanent liver damage. Some
infants with biliary atresia who undergo a successful Kasai
operation are restored to good health and can lead a normal life
without jaundice or major liver problems.
Drawing of the Kasai procedure for biliary atresia. Part of the
small intestine is attached to the liver and replaces the bile
ducts so the liver can drain properly.
The Kasai Procedure
Unfortunately, the Kasai procedure is not always successful. If
bile flow is not restored, the child will likely develop worsening
liver disease and cirrhosis and require liver transplantation
within the first 1 to 2 years of life. In addition, the Kasai
operation, even when initially successful, may not totally restore
normal liver development and function. A child with biliary
atresia may slowly develop cirrhosis and related complications and
require a liver transplant later in childhood.
While the Kasai procedure has been a great advance in the
management of biliary atresia, improvements in the operation and
clinical management of children who undergo it are needed to
improve the outcomes of children with this disease.
Liver Transplantation
Liver transplantation is a highly successful treatment for biliary
atresia and the survival rate after surgery has increased
dramatically in recent years. Children with biliary atresia are
now living into adulthood, some even having children of their own.
Because biliary atresia is not an inherited disease, the children
of survivors of biliary atresia do not have an increased risk of
having it themselves.
Improvements in transplant surgery have also led to a greater
availability of livers for transplantation in children with
biliary atresia. In the past, only livers from small children
could be used for a child with biliary atresia because the size of
the liver had to match. Recently, advanced methods have been
developed to use part of an adult’s liver, called “reduced size”
or “split liver” transplants, for transplant in a child with
biliary atresia.
In addition, surgery has been developed that allows taking part of
a living adult donor’s liver to use for transplantation. Thus,
parents or relatives of children with biliary atresia can donate a
part of their liver for transplantation. Because healthy liver
tissue grows quickly, if a child receives part of a liver from a
living donor, both the donor and the child can grow complete
livers over time.
What happens after surgery?
Both before and after the Kasai procedure, infants will receive a
specific diet with the right mix of nutrients and vitamins in a
form that does not require bile to be absorbed. Poor nutrition can
lead to problems with development, so doctors will monitor an
infant’s nutritional intake closely.
Some infants develop fluid in the abdomen after the Kasai
procedure, which makes the baby’s belly swell. This condition is
called ascites and usually only lasts for a few weeks. If ascites
lasts for more than 6 weeks, cirrhosis is likely present and the
infant will probably require a liver transplant.
Also common after the Kasai procedure is infection in the
remaining bile ducts inside the liver, called cholangitis. Doctors
may prescribe antibiotics to prevent cholangitis or prescribe them
once the infection occurs.
Children with biliary atresia may continue to have liver problems
after the Kasai procedure. Even with success of the operation and
return of bile flow, some children will develop injury and loss of
the small bile ducts inside the liver, which can cause scarring
and cirrhosis.
The liver affected by cirrhosis does not work well and is more
rigid and stiff than a normal liver. As a result, the blood flow
through the liver is slowed and under higher pressure. This
condition is called portal hypertension. Portal hypertension can
also cause flow of blood around, rather than through, the liver.
This complication can cause intestinal bleeding that may require
surgery and may eventually lead to a recommendation for liver
transplantation.
Cirrhosis of the liver can also lead to problems with nutrition,
bruising and bleeding, and itching skin. Itching, called pruritus,
is caused by the build up of bile in the blood and irritation of
nerve endings in the skin. Doctors may prescribe medications for
itching including resins that bind bile in the intestines or
antihistamines that decrease the skin’s sensation of itching.
|
|
|
Growing Stronger, Growing
Better
|
 |
| |
|
Global Health |
| |
 |
|
health checkup

|
|
Healthcare Provider |
| |


|
|
|
Biliary Atresia - treatment of Biliary Atresia,
Biliary Atresia types, Disease medicines, Biliary Atresia symptoms, Biliary
Atresia and Disease symptoms, Biliary Atresia symptoms Disease and
diagnosis, Symptoms and Solutions, Signs and Symptoms, type of Biliary
Atresia, cause common, common Biliary Atresia, Biliary Atresia List, causes
list, Infectious Biliary Atresia, Causes, Diseases , Types, Prevention,
Treatment and Facts, Biliary Atresia information, Biliary Atresia:
Definition, Biliary Atresia names, medical Biliary Atresia, medical Biliary
Atresia and disorders, cell Biliary Atresia, Biliary Atresia Worldwide,
Biliary Atresia Research, Biliary Atresia Control, Biliary Atresia Center,
Digestive Biliary Atresia Week, Information about Biliary Atresia, causes of
different Biliary Atresia, Biliary Atresia Articles, Biliary Atresia and
conditions, Health and Biliary Atresia, Biliary Atresia Patients, Biliary
Atresia and Sciences, causes of alzheimer's Biliary Atresia, Biliary Atresia
causes, alternative medicine heart Biliary Atresia, body ailments, Biliary
Atresia medicines, medical antiques, type of blood Biliary Atresia |
|
|