|
* Colon anatomy and development
* Malrotation
* Small bowel and colonic intussusception
* Fistulas
* Colonic atresia
* Volvulus
* Imperforate anus
* Hope through research
* Points to remember
* For more information
The colon, or large intestine, is part of the digestive system,
which is a series of organs from the mouth to the anus. When the
shape of the colon or the way it connects to other organs is
abnormal, digestive problems result. Some of these anatomic
problems can occur during embryonic development of the fetus in
the womb and are known as congenital abnormalities. Other problems
develop with age.
Colon Anatomy and Development
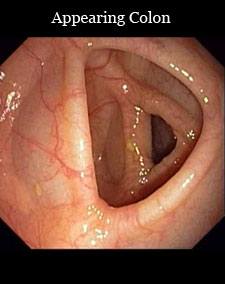
The adult colon is about 5 feet long. It connects to the small
bowel, which is also known as the small intestine. The major
functions of the colon are to absorb water and salts from
partially digested food that enters from the small bowel and then
send waste out of the body through the anus. What remains after
absorption is stool, which passes from the colon into the rectum
and out through the anus when a person has a bowel movement.
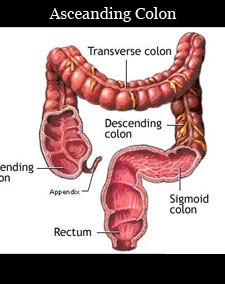
The colon comprises several segments:
* the cecum, the portion just after the small bowel
* the ascending colon
* the transverse colon
* the descending colon
* the sigmoid colon, an S-shaped portion near the end of the colon
* the rectum, where stool is stored until evacuation
The colon is formed during the first 3 months of embryonic
development. As the bowel lengthens, part of it passes into the
umbilical cord, which connects the fetus to the mother. As the
fetus grows and the abdominal cavity enlarges, the bowel returns
to the abdomen and turns, or rotates, counterclockwise to its
final position. The small bowel and colon are held in position by
tissue known as the mesentery. The ascending colon and descending
colon are fixed in place in the abdominal cavity. The cecum,
transverse colon, and sigmoid colon are suspended from the back of
the abdominal wall by the mesentery.
Anatomic Problems of the Colon
Malrotation and Volvulus
If the bowel does not rotate completely during embryonic
development, problems can occur. This condition is called
malrotation. Normally, the cecum is located in the lower right
part of the abdomen. If the cecum is not positioned correctly, the
bands of thin tissue that normally hold it in place may cross over
and block part of the small bowel.
Also, if the small bowel and colon have not rotated properly, the
mesentery may be only narrowly attached to the back of the
abdominal cavity. This narrow attachment can lead to a mobile or
floppy bowel that is prone to twisting, a disorder called volvulus.
(See the section on volvulus.)
Malrotation is also associated with other gastrointestinal (GI)
conditions, including Hirschsprung disease and bowel atresia.
Malrotation is usually identified in infants. About 60 percent of
these cases are found in the first month of life. Malrotation
affects both boys and girls, although boys are more often
diagnosed in infancy.
The colon is held in place by the mesentery
In malrotation, the cecum is not positioned correctly. The tissue
that normally holds it in place may cross over and block part of
the small bowel.
In infants, the main symptom of malrotation is vomiting bile. Bile
is a greenish-yellow digestive fluid made by the liver and stored
in the gallbladder. Symptoms of malrotation with volvulus in older
children include vomiting (but not necessarily vomiting bile),
abdominal pain, diarrhea, constipation, bloody stools, rectal
bleeding, or failure to thrive
Various imaging studies are used to diagnose malrotation:
* x rays to determine whether there is a blockage. In malrotation,
abdominal x rays commonly show that air, which normally passes
through the entire digestive tract, has become trapped. The
trapped air creates an enlarged, air-filled stomach and upper
small bowel, with little or no air in the rest of the small bowel
or the colon.
* upper GI series to locate the point of intestinal obstruction.
With this test, the patient swallows barium to coat the stomach
and small bowel before x rays are taken. Barium makes the organs
visible on x ray and indicates the point of the obstruction. This
test cannot be done if the patient is vomiting.
* lower GI series to determine the position of the colon. For this
test, a barium enema is given while x rays are taken. The barium
makes the colon visible so the position of the cecum can be
determined.
*computed tomography (CT) scan to help determine and locate the
intestinal obstruction.
Malrotation in infants is a medical emergency that usually
requires immediate surgery. Surgery may involve
* untwisting the colon
* dividing the bands of tissue that obstruct the small bowel
* repositioning the small bowel and colon
* removing the appendix
Surgery to relieve the blockage of the small bowel is usually
successful and allows the digestive system to function normally.
Small Bowel and Colonic Intussusception
Intussusception is a condition in which one section of the bowel
tunnels into an adjoining section, like a collapsible telescope.
Intussusception can occur in the colon, the small bowel, or
between the small bowel and colon. The result is a blocked small
bowel or colon.
Intussusception is rare in adults. Causes include
* benign or malignant growths
* adhesions (scarlike tissue)
* surgical scars in the small bowel or colon
* motility disorders (problems with the movement of food through
the digestive tract)
* long-term diarrhea
Some cases of intussusception have been associated with viral
infections and in patients living with AIDS. It can also occur
without any known cause (idiopathic).
In infants and children, intussusception involving the small bowel
alone, or the small bowel and the colon, is one of the most common
causes of intestinal obstruction. Malrotation is a risk factor.
Intussusception affects boys more often than girls, with most
cases happening at 5 months and at 3 years of age. Most cases in
children have no known cause, but viral infections or a growth in
the small bowel or colon may trigger the condition. In the past,
cases of intussusception appeared to be associated with a
childhood vaccine for rotavirus, a common cause of gastroenteritis
(intestinal infection). That vaccine is no longer given.
In adults with intussusception, symptoms can last a long time
(chronic symptoms) or they can come and go (intermittent
symptoms). The symptoms will depend on the location of the
intussusception. They may include
* changes in bowel habits
* urgency—needing to have a bowel movement immediately
* rectal bleeding
* chronic or intermittent crampy abdominal pain
* pain in a specific area of the abdomen
* abdominal distention
* nausea and vomiting
Children with intussusception may experience
* intermittent abdominal pain
* bowel movements that are mixed with blood and mucus
* abdominal distention or a lump in the abdomen
* vomiting bile
* diarrhea
* fever
* dehydration
* lethargy
* shock (low blood pressure, increased heart rate requiring
immediate attention)
If intussusception is not diagnosed promptly, especially in
children, it can cause serious damage to the portion of the bowel
that is unable to get its normal blood supply. A range of
diagnostic tests may be required. X rays of the abdomen may
suggest a bowel obstruction (blockage). Upper and lower GI series
will locate the intussusception and show the telescoping. CT scans
can also help with the diagnosis. When intussusception is
suspected, an air or barium enema can often help correct the
problem by pushing the telescoped section of bowel into its proper
position.
Both adults and children may require surgery to straighten or
remove the involved section of bowel. The outcome of this surgery
depends on the stage of the intussusception at diagnosis and the
underlying cause. With early treatment, the outcome is generally
excellent. In some cases, usually in children, intussusception may
be temporary and reverse on its own. If no underlying cause is
found in these cases, no specific treatment is required.
Fistulas
A fistula is an abnormal passageway between two areas of the
digestive tract. An internal fistula occurs between two areas of
intestine or an area of intestine and another organ. An external
fistula occurs between the intestine and the outside of the body.
Both internal and external fistulas may be characterized by
abdominal pain and swelling. External fistulas may discharge pus
or intestinal contents. Internal fistulas can be associated with
diarrhea.
The most common types of fistulas develop around the anus, colon,
and small bowel. These types are
* ileosigmoid—occurs between the sigmoid colon and the end of the
small bowel, which is also called the ileum
* ileocecal—occurs between the ileum and cecum
* anorectal—occurs between the anal canal and the skin around the
anus
* anovaginal—occurs between the rectum and vagina
* colovesical—occurs between the colon and bladder
* cutaneous—occurs between the colon or small bowel and the
outside of the body
Fistulas can occur at any age. Some fistulas are congenital, which
means they occur during the development of a baby. They are seen
in infants and are more common in boys. Other fistulas develop
suddenly due to diseases or after trauma, surgery, or local
infection. A fistula can form when diseased or damaged tissue
comes into contact with other damaged or nondamaged tissue, as
seen in Crohn's disease (intestinal inflammation) and
diverticulitis. Childbirth can lead to fistulas between the rectum
and vagina in women.
External fistulas are found during a physical examination.
Internal fistulas can be seen by colonoscopy, upper and lower GI
series, or CT scan.
Fistulas may be treated by surgery to remove the portion of the
intestine causing the fistula, along with antibiotics to treat any
associated infection.
Colonic Atresia
Colonic atresia is a condition that occurs during embryonic
development in which the normal tubular shape of the colon in the
fetus is unexpectedly closed. This congenital abnormality may be
caused by incomplete development of the colon or the loss of blood
flow during its development. Colonic atresia is rare and may occur
with the more common small bowel atresia.
Infants with colonic atresia have no bowel movements, increasing
abdominal distention, and vomiting. X rays will show a dilated
colon above the obstruction, which can then be located using a
barium enema.
Surgery is necessary to open or remove the closed area and
re-connect the normal sections of the colon.
Volvulus
Volvulus refers to the twisting of a portion of the intestine
around itself or a stalk of mesentery tissue to cause an
obstruction. Volvulus occurs most frequently in the colon,
although the stomach and small bowel can also twist. The part of
the digestive system above the volvulus continues to function and
may swell as it fills with digested food, fluid, and gas. A
condition called strangulation develops if the mesentery of the
bowel is twisted so tightly that blood flow is cut off and the
tissue dies. This condition is called gangrene. Volvulus is a
surgical emergency because gangrene can develop quickly, cause a
hole in the wall of the bowel (perforation), and become
life-threatening.
In the colon, volvulus most often involves the cecum and sigmoid
segment. Sigmoid volvulus is more common than cecal volvulus.
Sigmoid Volvulus
The sigmoid is the last section of the colon. Two anatomic
differences can increase the risk of sigmoid volvulus. One is an
elongated or movable sigmoid colon that is unattached to the left
sidewall of the abdomen. Another is a narrow mesentery that allows
twisting at its base. Sigmoid volvulus, however, can occur even
without an anatomic abnormality.
Risk factors that can make a person more likely to have sigmoid
volvulus are Hirschsprung disease, intestinal pseudo-obstructions,
and megacolon (an enlarged colon). Adults, children, and infants
can all have sigmoid volvulus. It is more common in men than in
women, possibly because men have longer sigmoid colons. It is also
more common in people over age 60, in African Americans, and in
institutionalized individuals who are on medications for
psychiatric disorders. In addition, children with malrotation are
more likely to get sigmoid volvulus.
The symptoms can be acute (occur suddenly) and severe. They
include a bowel obstruction (commonly seen in infants), nausea,
vomiting, bloody stools, abdominal pain, constipation, and shock.
Other symptoms can develop more slowly but increase over time,
such as severe constipation, lack of passing gas, crampy abdominal
pain, and abdominal distention. A doctor may also hear increased
or decreased bowel sounds.
Several tests are used to diagnose sigmoid volvulus. X rays show a
dilated colon above the volvulus. Upper and lower GI series help
locate the point of obstruction and show whether malrotation of
the rest of the colon is present. A CT scan may be used to show
the degree of twisting and malrotation, and whether perforation
has occurred.
In most instances, a sigmoidoscope, a tube used to look into the
sigmoid colon and rectum, can be used to reach the site, untwist
the colon, and release the obstruction. However, if the colon is
found to be twisted very tightly or is twisted so tightly that
blood flow is cut off and the tissue is dead, immediate surgery
will be needed to correct the problem and, if possible, restore
the blood supply. Dead tissue will be removed during surgery, and
a portion of the colon may be removed as well—a procedure called a
resection. Sigmoid volvulus can recur after untwisting with the
sigmoidoscope, but resection eliminates the chance of recurrence.
Prompt diagnosis of sigmoid volvulus and appropriate treatment
generally lead to a good outcome.
Cecal Volvulus
Cecal volvulus is the twisting of the cecum and ascending segment
of the colon. Normally, the cecum and ascending colon are fixed to
the internal abdominal wall. If not, they can move and become
twisted. The main symptoms of cecal volvulus are crampy abdominal
pain and swelling that are sometimes associated with nausea and
vomiting.
In testing, x rays will show the cecum out of its normal place and
inflated with trapped air. The appendix may be filled with gas,
but little or no gas is seen in other parts of the colon. Upper
and lower GI series will locate the volvulus and the position of
the colon. A CT scan may show how tightly the volvulus is twisted.
A colonoscopy, which uses a small, flexible tube with a light and
a lens on the end to see the inside of the colon, can sometimes be
used to untwist the volvulus. If the cecum becomes gangrenous or
holes develop in it, surgery will be needed.
|