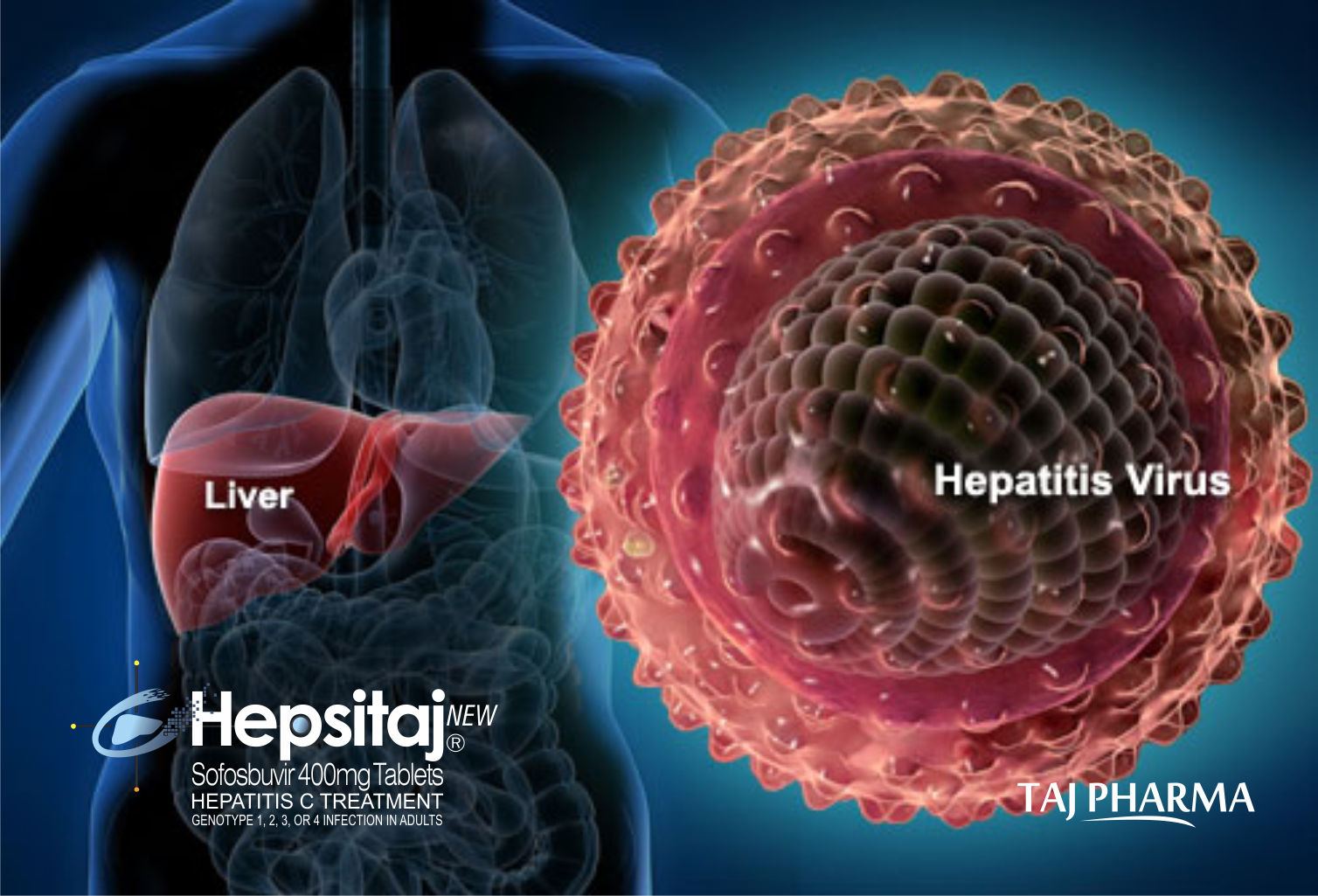
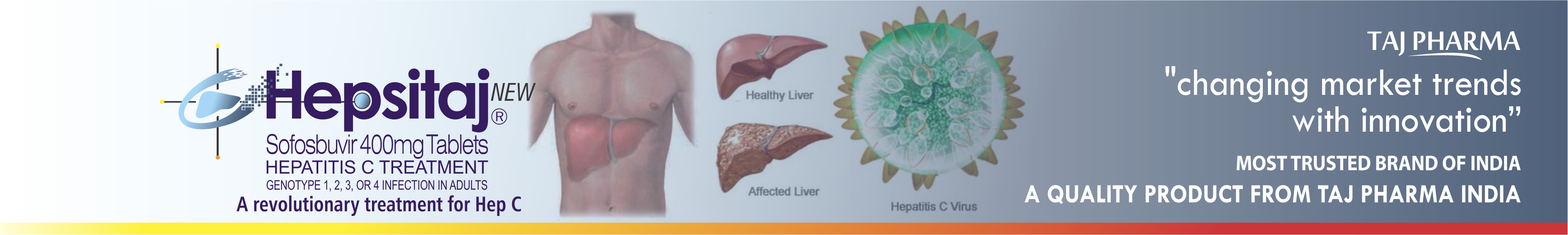
HEPSITAJ OFFERS HOPE THAT YOU CAN PUT HEPATITIS C (HEP C)
BEHIND YOU. HEPSITAJ IS A PRESCRIPTION MEDICINE USED WITH OTHER
ANTIVIRAL MEDICINES TO TREAT CHRONIC (LASTING A LONG TIME)
HEPATITIS C GENOTYPE 1, 2, 3, OR 4 INFECTION IN ADULTS. IT
IS NOT KNOWN IF HEPSITAJ IS SAFE AND EFFECTIVE IN CHILDREN
UNDER 18 YEARS OF AGE.
HEPSITAJ IS A PRESCRIPTION MEDICINE USED WITH OTHER ANTIVIRAL
MEDICINES TO TREAT CHRONIC (LASTING A LONG TIME) HEPATITIS C
GENOTYPE 1, 2, 3, OR 4 INFECTION IN ADULTS.
IT IS NOT KNOWN IF HEPSITAJ IS SAFE AND EFFECTIVE IN CHILDREN
UNDER 18 YEARS OF AGE. WITH HEPSITAJ, THERE’S HOPE THAT YOU CAN
PUT HEP C BEHIND YOU. YOU MAY BE ABLE TO STOP THINKING ABOUT
YOUR DISEASE, TAKE THE NEXT STEP, AND SET A NEW COURSE.
HEPSITAJ Tablets (Sofosbuvir )
HEPSITAJ TABLETS
EACH FILM-COATED TABLET
CONTAINS:
SOFOSBUVIR ……………………………400
MG
COLOURS: RED OXIDE OF
IRON & TITANIUM DIOXIDE USP
HEPSITAJ- A.T* TABLETS
EACH TABLET CONTAINS:
LEDIPASVIR
…………………………………..90 MG
SOFOSBUVIR………………......……………400 MG
EXCIPIENTS...................................................Q.S.
COLOURS: FERRIC OXIDE USP-NF
RED, FERRIC OXIDE USP-NF YELLOW & TITANIUM DIOXIDE USP.
*ADVANCE TREATMENTS.
Tablet
Pharmacodynamics
Mechanism of Action
Sofosbuvir is a direct-acting antiviral (DAA)
agent against the hepatitis C virus (HCV). It is an inhibitor of
the HCV NS5B RNA-dependent RNA polymerase, which is essential
for viral replication. Sofosbuvir is a nucleotide prodrug that
undergoes intracellular metabolism to form a pharmacologically
active uridine analog triphosphate (GS-461203), which can be
incorporated into HCV RNA by the NS5B polymerase and acts as a
chain terminator.
Effect on Electrocardiogram
The effect of sofosbuvir 400 and 1,200 mg on the
QTc interval was evaluated in a randomized, single-dose,
placebo- and active-controlled (moxifloxacin 400 mg) four-period
crossover through a QT trial in 59 healthy subjects. At a dose
three times the maximum recommended dose, sofosbuvir does not
prolong QTc to any clinically relevant extent.
Pharmacokinetics
Absorption
The pharmacokinetic properties of sofosbuvir and
its predominant circulating metabolite (GS-331007) have been
evaluated in healthy adult subjects and in subjects with chronic
hepatitis C. Following oral administration, sofosbuvir was
absorbed with a peak plasma concentration observed at ~0.5–2
hours post-dose, regardless of dose level. Peak plasma
concentration of the metabolite was observed between 2 and 4
hours post-dose. Based on population pharmacokinetic analysis in
subjects with genotype 1–6 HCV infection who were
co-administered ribavirin (with or without pegylated
interferon), the geometric mean, steady-state AUC0–24 of
sofosbuvir (N=838) and GS-331007 (N=1.695) were 828 ng.hr/mL and
6,790 ng.hr/mL, respectively. Relative to healthy subjects
administered sofosbuvir alone (N = 272), the sofosbuvir AUC0–24 was
39% higher and, GS-331007 AUC0–24 was
39% lower, respectively, in HCV-infected subjects. Sofosbuvir
and GS-331007 AUCs are near dose-proportional over the dose
range of 200 mg to 1,200 mg.
Effect of Food
Relative to fasting conditions, the
administration of a single dose of sofosbuvir with a
standardized high-fat meal did not substantially affect the
sofosbuvir Cmax or
AUC0–inf. The exposure of
GS-331007 was not altered in the presence of a high-fat meal.
Therefore, sofosbuvir can be administered without regard to
food.
Distribution
Sofosbuvir is approximately 61–65% bound to human
plasma proteins and the binding is independent of drug
concentration over the range of 1 μg/mL to 20 μg/mL. Protein
binding of the sofosbuvir metabolite was minimal in human
plasma. After a single 400 mg dose of -sofosbuvir in healthy
subjects, the blood to plasma ratio of 14C-radioactivity
was approximately 0.7.
Metabolism
Sofosbuvir is extensively metabolized in the
liver to form a pharmacologically active nucleoside analog
triphosphate GS-461203. The metabolic activation pathway
involves sequential hydrolysis of the carboxyl ester moiety
catalyzed by human cathepsin A (CatA) or carboxylesterase 1
(CES1) and phosphoramidate cleavage by histidine triad
nucleotide-binding protein 1 (HINT1) is followed by
phosphorylation by the pyrimidine nucleotide biosynthesis
pathway. Dephosphorylation results in the formation of a
nucleoside metabolite, GS-331007, that cannot be efficiently
rephosphorylated and lacks anti-HCV activity in
vitro.
After a single 400 mg oral dose of -sofosbuvir,
sofosbuvir and GS-331007 accounted for approximately 4% and >90%
of drug-related material (sum of molecular weight-adjusted AUC
of sofosbuvir and its metabolites) systemic exposure,
respectively.
Excretion
Following a single 400 mg oral dose of -sofosbuvir,
mean total recovery of the dose was greater than 92%, consisting
of approximately 80%, 14%, and 2.5% recovered in urine, feces,
and expired air, respectively. The majority of the sofosbuvir
dose recovered in urine was GS-331007 (78%) while 3.5% was
recovered as sofosbuvir. These data indicate that renal
clearance is the major elimination pathway for the metabolite.
The median terminal half-lives of sofosbuvir and GS-331007 were
0.4 and 27 hours, respectively.
Special Populations
Gender
No clinically relevant pharmacokinetic
differences have been observed between men and women for
sofosbuvir and GS-331007.
Race
Population pharmacokinetics analysis in HCV-infected
subjects indicated that race had no clinically relevant effect
on the exposure of sofosbuvir and GS-331007.
Geriatric
Population pharmacokinetic analysis in HCV-infected
subjects showed that within the age range (19 to 75 years)
analyzed, age did not have a clinically relevant effect on the
exposure to sofosbuvir and GS-331007 .
Pediatric
The pharmacokinetics of sofosbuvir in pediatric
patients has not been established.
Renal Impairment
The pharmacokinetics of sofosbuvir were studied
in HCV-negative subjects with mild (eGFR ≥50 and <80 mL/min/1.73m2),
moderate (eGFR ≥30 and <50 mL/ min/ 1.73 m 2),
severe renal impairment (eGFR <30 mL/min/1.73m2)
and subjects with end-stage renal disease (ESRD) requiring
hemodialysis following a single 400 mg dose of sofosbuvir.
Relative to subjects with normal renal function (eGFR >80 mL/
min /1.73m2), the sofosbuvir
AUC0-inf was
61%, 107% and 171% higher in mild, moderate and severe renal
impairment, while the GS-331007 AUC0–inf was
55%, 88% and 451% higher, respectively. In subjects with ESRD,
relative to subjects with normal renal function, sofosbuvir and
GS-331007 AUC0–inf was
28% and 1,280% higher when sofosbuvir was dosed 1 hour before
hemodialysis compared with 60% and 2,070% higher when sofosbuvir
was dosed 1 hour after hemodialysis, respectively. A 4-hour
hemodialysis session removed approximately 18% of the
administered dose. No dose adjustment is required for patients
with mild or moderate renal impairment. The safety and efficacy
of sofosbuvir has not been established in patients with severe
renal impairment or ESRD. No dose recommendation can be given
for patients with severe renal impairment or ESRD .
Hepatic Impairment
The pharmacokinetics of sofosbuvir was studied
following a 7-day dosing of 400 mg sofosbuvir in HCV-infected
subjects with moderate and severe hepatic impairment (Child-Pugh
class B and C). Relative to subjects with normal hepatic
function, the sofosbuvir AUCs0–24 were
126% and 143% higher in moderate and severe hepatic impairment
while the GS-331007 AUCs0–24 were
18% and 9% higher, respectively. Population pharmacokinetics
analysis in HCV-infected subjects indicated that cirrhosis had
no clinically relevant effect on the exposure of sofosbuvir and
GS-331007. No dose adjustment of sofosbuvir is recommended for
patients with mild, moderate and severe hepatic impairment .
HEPSITAJ Tablets,
which contain sofosbuvir, a HCV nucleotide analog NS5B
polymerase inhibitor, are indicated in combination with under
medicinal products for the treatment of chronic hepatitis C (CHC)
in adults.
Sofosbuvir efficacy has been established in
subjects with HCV genotype 1, 2, 3 or 4 infection, including
those with hepatocellular carcinoma meeting Milan criteria
(awaiting liver transplantation) and those with HCV/HIV-1
co-infection .
The following points should be considered when
initiating treatment with HEPSITAJ
Tablets:
·
Monotherapy of sofosbuvir is not recommended for
treatment of CHC.
·
Treatment regimen and duration are dependent on
both viral genotype and patient population .
·
Treatment response varies based on baseline host
and viral factors .
The recommended dose of HEPSITAJ
Tablets is
one 400 mg tablet, taken orally, once daily with or without food .
Sofosbuvir should be used in combination with
ribavirin or in combination with pegylated (peg)-interferon alfa
and ribavirin for the treatment of CHC in adults. The
recommended regimen and treatment duration for sofosbuvir
combination therapy is provided in Table 1.
Table 1: Recommended regimens and treatment
duration for sofosbuvir combination therapy in HCV mono-infected
and HCV/HIV-1 co-infected patients
|
|
Treatment |
Duration |
|
Patients with genotype 1 or 4 CHC |
Sofosbuvir+ peg-interferon alfaa +
ribavirinb |
12 weeks |
|
Patients with genotype 2 CHC |
Sofosbuvir + ribavirinb |
12 weeks |
|
Patients with genotype 3 CHC |
Sofosbuvir + ribavirinb |
24 weeks |
a See
peg-interferon alfa prescribing information for dosing
recommendation for patients with genotype 1 or 4 CHC.
b Dose
of ribavirin is weight-based (<75 kg = 1,000 mg and ≥75 kg =
1,200 mg). The daily dose of ribavirin is administered orally in
two divided doses with food. Patients with renal impairment (CrCl
≤50 mL/min) require ribavirin dose reduction; refer to ribavirin
prescribing information.
Sofosbuvir in combination with ribavirin for 24
weeks can be considered as a therapeutic option for CHC patients
with genotype 1 infection who are ineligible to receive an
interferon-based regimen . Treatment decision should be guided
by an assessment of the potential benefits and risks for the
individual patient.
Patients with Hepatocellular Carcinoma Awaiting
Liver Transplantation
Sofosbuvir in combination with ribavirin is
recommended for up to 48 weeks or until the time of liver
transplantation, whichever occurs first, to prevent
post-transplant HCV reinfection .
Dose Modification
Dose reduction of sofosbuvir is not recommended.
Genotypes 1 and 4
If a patient has a serious adverse reaction
potentially related to peg-interferon alfa and/or ribavirin, the
peg-interferon alfa and/or ribavirin dose should be reduced or
discontinued. Refer to the peg-interferon alfa and ribavirin
prescribing information for additional information about how to
reduce and/or discontinue the peg-interferon alfa and/or
ribavirin dose.
Genotypes 2 and 3
If a patient has a serious adverse reaction
potentially related to ribavirin, the ribavirin dose should be
modified or discontinued, if appropriate, until the adverse
reaction abates or decreases in severity. Table 2 provides
guidelines for dose modifications and discontinuation based on
the patient’s hemoglobin concentration and cardiac status.
Table 2: Ribavirin dose modification guideline
for co-administration with sofosbuvir
a The
daily dose of ribavirin is administered orally in two divided
doses with food.
b Once
ribavirin has been withheld due to either a laboratory
abnormality or clinical manifestation, an attempt may be made to
restart ribavirin at 600 mg daily and further increase the dose
to 800 mg daily. However, it is not recommended that ribavirin
be increased to the original assigned dose (1,000 mg to 1,200 mg
daily).
Discontinuation of Dosing
If the other agents used in combination with
sofosbuvir are permanently discontinued, sofosbuvir should also
be discontinued.
Severe Renal Impairment and ESRD
No dose recommendation can be given for patients
with severe renal impairment (estimated glomerular filtration
rate <30 mL/min/1.73 m2) or
with ESRD due to higher exposures (up to 20-fold) of the
predominant sofosbuvir metabolite .
When sofosbuvir is used in combination with
ribavirin or peg-interferon alfa/ribavirin, the
contraindications applicable to those agents are applicable to
combination therapies. Refer to the prescribing information of
peg-interferon alfa and ribavirin for a list of their
contraindications.
Drug Interactions
Potential for Drug Interactions
After oral administration of sofosbuvir, it is
rapidly converted to the predominant circulating metabolite,
GS-331007, that accounts for greater than 90% of drug related
material systemic exposure, whereas the parent sofosbuvir
accounts for approximately 4% of drug-related material . In
clinical pharmacology studies, both sofosbuvir and GS-331007
were monitored for purposes of pharmacokinetic analyses.
Sofosbuvir is a substrate of the drug
transporter, P-gp, and the breast cancer resistance protein (BCRP)
while GS-331007 is not. Drugs that are potent P-gp inducers in
the intestine (e.g., rifampin or St. John’s Wort) may decrease
sofosbuvir plasma concentrations, leading to a reduced
therapeutic effect of sofosbuvir and, thus, should not be used
with sofosbuvir . Co-administration
of sofosbuvir with drugs that inhibit P-gp and/or BCRP may
increase the sofosbuvir plasma concentration without increasing
the GS-331007 plasma concentration; accordingly, sofosbuvir may
be co-administered with P-gp and/or BCRP inhibitors. Sofosbuvir
and GS-331007 are not inhibitors of P-gp and BCRP and, thus, are
not expected to increase exposures of drugs that are substrates
of these transporters.
The intracellular metabolic activation pathway of
sofosbuvir is mediated by generally low-affinity and
high-capacity hydrolase and nucleotide phosphorylation pathways
that are unlikely to be affected by concomitant drugs .
Potentially Significant Drug Interactions
Drug interaction information for sofosbuvir with
potential concomitant drugs is summarized in Table 3. The drug
interactions described are based on potential drug interactions
that may occur with sofosbuvir. The table is not all-inclusive .
Table 3: Potentially significant drug
interactions: Alteration in dose or regimen may be recommended
based on drug interaction studies or predicted interactiona
|
Concomitant Drug Class: Drug Name |
Effect on Concentrationb |
Clinical Comment |
|
Anti-arrhythmics:
Amiodarone
|
Effect on
amiodarone and sofosbuvir
concentrations unknown
|
Co-administration of amiodarone with
sofosbuvir in combination with another DAA may result in
serious symptomatic bradycardia. The mechanism of this
effect is unknown. Co-administration of amiodarone with
sofosbuvir in combination with another DAA is not
recommended; if co-administration is required, cardiac
monitoring is recommended
|
|
Anticonvulsants: Carbamazepine
Phenytoin Phenobarbital Oxcarbazepine |
↓ sofosbuvir
↓ GS-331007 |
Co-administration of sofosbuvir with
carbamazepine, phenytoin, phenobarbital or oxcarbazepine
is expected to decrease the concentration of sofosbuvir,
leading to reduced therapeutic effect of sofosbuvir.
Co-administration is not recommended. |
|
Antimycobacterials: Rifabutin
Rifampin
Rifapentine |
↓ sofosbuvir
↓ GS-331007 |
Co-administration of sofosbuvir with
rifabutin or rifapentine is expected to decrease the
concentration of sofosbuvir, leading to reduced
therapeutic effect of sofosbuvir. Co-administration is
not recommended. Sofosbuvir should not be used with
rifampin, a potent intestinal P-gp inducer. |
|
Herbal Supplements: St.
John’s Wort (Hypericum
perforatum) |
↓ sofosbuvir
↓ GS-331007 |
Sofosbuvir should not be used with St.
John’s Wort, a potent intestinal P-gp inducer. |
|
HIV Protease Inhibitors: Tipranavir/ritonavir |
↓ sofosbuvir
↓ GS-331007 |
Co-administration of sofosbuvir with
tipranavir/ritonavir is expected to decrease the
concentration of sofosbuvir, leading to reduced
therapeutic effect of sofosbuvir. Co-administration is
not recommended. |
a This
table is not all-inclusive.
b ↓
= decrease.
Drugs without Clinically Significant Interactions
with Sofosbuvir
In addition to the drugs included in Table 3, the
interaction between sofosbuvir and the following drugs was
evaluated in clinical trials and no dose adjustment is needed
for either drug : cyclosporine, darunavir/ritonavir, efavirenz,
emtricitabine, methadone, raltegravir, rilpivirine, tacrolimus,
or tenofovir disoproxil fumarate.
Use with Potent P-gp Inducers
Drugs that are potent P-gp inducers in the
intestine (e.g. rifampin, St. John’s Wort) may significantly
decrease sofosbuvir plasma concentrations and may lead to a
reduced therapeutic effect of sofosbuvir. Rifampin and St.
John’s wort should not be used with sofosbuvir .
Serious Symptomatic Bradycardia When
Co-administered with Amiodarone and another HCV DAA
Postmarketing cases of symptomatic bradycardia
and cases requiring pacemaker intervention have been reported
when amiodarone is co-administered with sofosbuvir in
combination with an investigational agent (NS5A inhibitor) or
simeprevir. A fatal cardiac arrest was reported in a patient
receiving a sofosbuvir-containing regimen (ledipasvir/
sofosbuvir). Bradycardia has generally occurred within hours to
days, but cases have been observed up to 2 weeks after
initiating HCV treatment. Patients also taking beta-blockers, or
those with underlying cardiac comorbidities and/or advanced
liver disease may be at increased risk for symptomatic
bradycardia with co-administration of amiodarone. Bradycardia
generally resolved after discontinuation of HCV treatment. The
mechanism for this effect is unknown.
Co-administration of amiodarone with sofosbuvir
in combination with another DAA is not recommended. For patients
taking amiodarone who have no other alternative, viable
treatment options and who will be co-administered sofosbuvir and
another DAA:
·
Counsel patients about the risk of serious
symptomatic bradycardia.
·
Cardiac monitoring in an in-patient setting for
the first 48 hours of co-administration is recommended, after
which outpatient or self-monitoring of the heart rate should
occur on a daily basis through at least the first 2 weeks of
treatment.
Patients who are taking sofosbuvir in combination
with another DAA who need to start amiodarone therapy due to no
other alternative, viable treatment options should undergo
similar cardiac monitoring as outlined above. Due to
amiodarone’s long half-life, patients discontinuing amiodarone
just prior to starting sofosbuvir in combination with a DAA
should also undergo similar cardiac monitoring as outlined
above.
Patients who develop signs or symptoms of
bradycardia should seek medical evaluation immediately. Symptoms
may include near-fainting or fainting, dizziness or
lightheadedness, malaise, weakness, excessive tiredness,
shortness of breath, chest pains, confusion or memory problems .
Risk of Reduced Therapeutic Effect Due to Use
with P-gp Inducers
Drugs that are P-gp inducers in the intestine
(e.g., rifampin, St. John’s wort) may significantly decrease
sofosbuvir plasma concentrations and may lead to a reduced
therapeutic effect of sofosbuvir. The use of rifampin and St.
John’s wort with sofosbuvir is not recommended .
Risks Associated with Combination Treatment
Because sofosbuvir is used in combination with
other antiviral drugs for treatment of HCV infection, consult
the prescribing information for these drugs used in combination
with sofosbuvir. Warnings and Precautions related to these drugs
also apply to their use in sofosbuvir combination treatment.
Related Products Not Recommended
The use of HEPSITAJ with
other products containing sofosbuvir is not recommended.
Patients with Hepatocellular Carcinoma
Awaiting Liver Transplantation
Sofosbuvir was studied in HCV-infected subjects
with hepatocellular carcinoma prior to undergoing liver
transplantation in an open-label clinical trial evaluating the
safety and efficacy of sofosbuvir and ribavirin administered
pre-transplant to prevent post-transplant HCV reinfection. The
primary endpoint of the trial was post-transplant virologic
response (pTVR) defined as HCV RNA less than the lower limit of
quantification (LLOQ) at 12 weeks post-transplant. HCV-infected
subjects, regardless of genotype, with hepatocellular carcinoma
meeting the MILAN criteria (defined as the presence of a tumor,
5 cm or less in diameter, in patients with single hepatocellular
carcinomas and no more than three tumor nodules, each 3 cm or
less in diameter, in patients with multiple tumors and no
extrahepatic manifestations of the cancer or evidence of
vascular invasion of tumor) received 400 mg sofosbuvir and
weight-based 1,000–1,200 mg ribavirin daily for 24–48 weeks or
until the time of liver transplantation, whichever occurred
first. An interim analysis was conducted on 61 subjects who
received sofosbuvir and ribavirin; 45 subjects had HCV genotype
1; 44 subjects had a baseline CPT score less than 7, and all
subjects had a baseline unadjusted MELD score ≤14. Of these 61
subjects, 41 subjects underwent liver transplantation following
up to 48 weeks of treatment with sofosbuvir and ribavirin; 37
had HCV RNA less than the LLOQ at the time of transplantation.
Of the 37 subjects, the post-transplant virologic response (pTVR)
rate was 64% (23/36) in the 36 evaluable subjects who had
reached the 12 week post-transplant time point. The safety
profile of sofosbuvir and ribavirin in HCV-infected subjects
prior to liver transplantation was comparable to that observed
in subjects treated with sofosbuvir and ribavirin in Phase 3
clinical trials.
Post-Liver Transplant Patients
The safety and efficacy of sofosbuvir has not
been established in post-liver transplant patients.
CHC Patients with Genotype 5 or 6 HCV
Infection
Available data on subjects with genotype 5 or 6
HCV infection are insufficient for dosing recommendations.
Renal Impairment
No dose adjustment of sofosbuvir is required for
patients with mild or moderate renal impairment. The safety and
efficacy of sofosbuvir have not been established in patients
with severe renal impairment (eGFR <30 mL/min/1.73 m2)
or ESRD requiring hemodialysis. No dose recommendation can be
given for patients with severe renal impairment or ESRD . Refer
also to ribavirin and peg-interferon alfa prescribing
information for patients with CrCl <50 mL/min.
Hepatic Impairment
No dose adjustment of sofosbuvir is required for
patients with mild, moderate or severe hepatic impairment
(Child-Pugh class A, B or C) . Safety and efficacy of sofosbuvir
have not been established in patients with decompensated
cirrhosis. See peg-interferon alfa prescribing information for
contraindication in hepatic decompensation.
Pregnancy
Pregnancy Category X: Use with Ribavirin or
Peg-interferon Alfa/Ribavirin
Ribavirin may cause birth defects and/or death of
the exposed fetus and animal studies have shown that interferons
have abortifacient effects. Extreme care must be taken to avoid
pregnancy in female patients and in female partners of male
patients. Ribavirin therapy should not be started unless a
report of a negative pregnancy test has been obtained
immediately prior to initiation of therapy.
When sofosbuvir is used in combination with
ribavirin or peg-interferon alfa/ribavirin, women of
childbearing potential and their male partners must use two
forms of effective contraception during treatment and for at
least 6 months after treatment has concluded. Routine monthly
pregnancy tests must be performed during this time. There are no
data on the effectiveness of systemic hormonal contraceptives in
women taking sofosbuvir; therefore, two non-hormonal methods of
contraception should be used during treatment with sofosbuvir
and concomitant ribavirin .
Significant teratogenic and/or embryocidal
effects have been demonstrated in all animal species exposed to
ribavirin; and, therefore, ribavirin is contraindicated in women
who are pregnant and in the male partners of women who are
pregnant . Interferons have abortifacient effects in animals and
should be assumed to have abortifacient potential in humans .
Pregnancy Category B: Sofosbuvir
There are no adequate and well-controlled studies
with sofosbuvir in pregnant women.
Lactation
It is not known whether sofosbuvir and its
metabolite(s) are present in human breast milk. The predominant
circulating metabolite (GS-331007) was the primary component
observed in the milk of lactating rats, without effect on the
nursing pups. Because of the potential for adverse reactions
from the drug in nursing infants, a decision must be made
whether to discontinue nursing or discontinue treatment with
ribavirin-containing regimens, taking into account the
importance of the therapy to the mother. Also see the
prescribing information for ribavirin.
Pediatric Use
Safety and effectiveness of sofosbuvir in
children less than 18 years of age have not been established.
Geriatric Use
Sofosbuvir was administered to 90 subjects aged
65 years and over. The response rates observed for subjects over
65 years of age were similar to that of younger subjects across
treatment groups. No dose adjustment of sofosbuvir is warranted
in geriatric patients .
Clinical Trials Experience
Sofosbuvir should be administered with ribavirin
or peg-interferon alfa/ribavirin. Refer to the prescribing
information of peg-interferon alfa and ribavirin for a
description of adverse reactions associated with their use.
Because clinical trials are conducted under
widely varying conditions, adverse reaction rates observed in
the clinical trials of a drug cannot be directly compared to
rates in the clinical trials of another drug and may not reflect
the rates observed in practice.
The safety assessment of sofosbuvir is based on
pooled Phase 3 clinical trial data (both controlled and
uncontrolled) including 650 subjects who received the sofosbuvir
+ ribavirin combination therapy for 12 weeks, 98 subjects who
received sofosbuvir + ribavirin combination therapy for 16
weeks, 250 subjects who received sofosbuvir + ribavirin
combination therapy for 24 weeks, 327 subjects who received
sofosbuvir + peg-interferon alfa + ribavirin combination therapy
for 12 weeks, 243 subjects who received peg-interferon alfa +
ribavirin for 24 weeks, and 71 subjects who received placebo for
12 weeks.
The proportion of subjects who permanently
discontinued treatment due to adverse events was 4% for subjects
receiving placebo, 1% for subjects receiving sofosbuvir +
ribavirin for 12 weeks, <1% for subjects receiving sofosbuvir +
ribavirin for 24 weeks, 11% for subjects receiving
peg-interferon alfa + ribavirin for 24 weeks, and 2% for
subjects receiving sofosbuvir + peg-interferon alfa + ribavirin
for 12 weeks.
Treatment-emergent adverse events observed in
≥15% of subjects in clinical trials are provided in Table 4. A
side-by-side tabulation is to simplify presentation; direct
comparison across trials should not be made due to differing
trial designs.
The most common adverse events (≥20%) for the
sofosbuvir + ribavirin combination therapy were fatigue and
headache. The most common adverse events (≥20%) for the
sofosbuvir + peg-interferon alfa + ribavirin combination therapy
were fatigue, headache, nausea, insomnia and anemia.
Less Common Adverse Reactions Reported in
Clinical Trials (<1%):
The following adverse events occurred in <1% of
subjects receiving sofosbuvir in a combination regimen in any
one trial. These events have been included because of their
seriousness or assessment of potential causal relationship.
Hematologic Effects: Pancytopenia
(particularly in subjects receiving concomitant peg-interferon).
Psychiatric Disorders:
Severe depression (particularly in subjects with pre-existing
history of psychiatric illness), including suicidal ideation and
suicide.
Peg-IFN=peg-interferon; RBV=ribavirin; PBO=placebo
a Subjects
received weight-based ribavirin (1,000 mg per day if weighing
<75 kg or 1,200 mg per day if weighing ≥75 kg).
b Subjects
received 800 mg ribavirin per day regardless of weight.
Bilirubin Elevations
Total bilirubin elevation of more than 2.5×ULN
was observed in none of the subjects in the 12 week sofosbuvir +
peg-interferon alfa + ribavirin group and in 1%, 3% and 3% of
subjects in the 24 weeks’ peg-interferon alfa + ribavirin, 12
weeks’ sofosbuvir + ribavirin and sofosbuvir + ribavirin 24
weeks’ groups, respectively. Bilirubin levels peaked during the
first 1–2 weeks of treatment and subsequently decreased and
returned to baseline levels by post-treatment week 4. These
bilirubin elevations were not associated with transaminase
elevations.
Creatine Kinase Elevations
Creatine kinase was assessed in the FISSION and
NEUTRINO trials. Isolated, asymptomatic creatine kinase
elevation of greater than or equal to 10×ULN was observed in
<1%, 1% and 2% of subjects in the peg-interferon alfa +
ribavirin 24 weeks’, sofosbuvir + peg-interferon alfa +
ribavirin 12 weeks’ and sofosbuvir + ribavirin 12 weeks’ groups,
respectively.
Lipase Elevations
Isolated, asymptomatic lipase elevation of
greater than 3×ULN was observed in <1%, 2%, 2%, and 2% of
subjects in the sofosbuvir + peg-interferon alfa + ribavirin 12
weeks’, sofosbuvir + ribavirin 12 weeks’, sofosbuvir + ribavirin
24 weeks’ and peg-interferon alfa + ribavirin 24 weeks’ groups,
respectively.
Patients with HCV/HIV-1 Co-infection
Sofosbuvir used in combination with ribavirin was
assessed in 223 HCV/HIV-1 co-infected subjects. The safety
profile in HCV/HIV-1 co-infected subjects was similar to that
observed in HCV mono-infected subjects. Elevated total bilirubin
(grade 3 or 4) was observed in 30/32 (94%) subjects receiving
atazanavir as part of the antiretroviral regimen. None of the
subjects had concomitant transaminase increases. Among subjects
not taking atazanavir, grade 3 or 4 elevated total bilirubin was
observed in 2 (1.5%) subjects, similar to the rate observed with
HCV mono-infected subjects receiving sofosbuvir+ ribavirin in
Phase 3 trials.
Postmarketing Experience
The following adverse reactions have been
identified during post-approval use of sofosbuvir. Because
postmarketing reactions are reported voluntarily from a
population of uncertain size, it is not always possible to
reliably estimate their frequency or establish a causal
relationship to drug exposure.
Cardiac Disorders: Serious
symptomatic bradycardia has been reported in patients taking
amiodarone who initiate treatment with sofosbuvir in combination
with another HCV direct acting antiviral .
The highest documented dose of sofosbuvir was a
single supra therapeutic dose of sofosbuvir 1,200 mg
administered to 59 healthy subjects. In that trial, there were
no untoward effects observed at this dose level, and adverse
events were similar in frequency and severity to those reported
in the placebo and sofosbuvir 400 mg treatment groups. The
effects of higher doses are not known.
No specific antidote is available for overdose
with sofosbuvir. If overdose occurs, the patient must be
monitored for evidence of toxicity. Treatment of overdose with
sofosbuvir consists of general supportive measures, including
monitoring of vital signs as well as observation of the clinical
status of the patient. A 4-hour hemodialysis session removed 18%
of the administered dose.
Store protected from moisture at a temperature
not exceeding 30°C.
HEPSITAJ
Tablets are
available in a plastic container of 14 tablets.
HEPSITAJ
Tablets are
available in a plastic container of 28 tablets.
HEPSITAJ-
A.T* Tablets
are available in plastic container of 10 & 30
tablets. |

 Hepatitis
B and C >Sovaldi (sofosbuvir) tablets for Sovaldi 400 mg
film-coated tablets
HEPSITAJ Tablets (Sofosbuvir ), sofosbuvir 400 mg tablet price,
sofosbuvir price, sofosbuvir in india, sofosbuvir ledipasvir, sofosbuvir
velpatasvir, sofosbuvir side effects, sovaldi price in India, sofosbuvir
mechanism of action, sofosbuvir tablets,
sofosbuvir
medication, Trade names: Sovaldi, Soforal, others, Sofosbuvir Tablets,
Learn about indications, dosage and how it is supplied for the drug Sovaldi
(
Hepatitis
B and C >Sovaldi (sofosbuvir) tablets for Sovaldi 400 mg
film-coated tablets
HEPSITAJ Tablets (Sofosbuvir ), sofosbuvir 400 mg tablet price,
sofosbuvir price, sofosbuvir in india, sofosbuvir ledipasvir, sofosbuvir
velpatasvir, sofosbuvir side effects, sovaldi price in India, sofosbuvir
mechanism of action, sofosbuvir tablets,
sofosbuvir
medication, Trade names: Sovaldi, Soforal, others, Sofosbuvir Tablets,
Learn about indications, dosage and how it is supplied for the drug Sovaldi
(


.png)